Measuring our performance
Outcomes, services and key performance indicators (KPIs) are used to measure the performance of the WA Health system. These measurements are used to assess the effectiveness and efficiency of the services delivered against agreed State Government priorities and desired outcomes.
The NMHS, as a health service provider, is responsible for delivering and reporting against outcomes and services including, but not limited to, the following:
Hospital-acquired complications – Pressure injury
A pressure injury is a sore, break or blister of the skin caused by unrelieved pressure or friction on an area of the body over time. The depth of skin damage can vary from shallow to very deep. Pressure injuries can be very painful and take a long time to heal. They may also reduce a patient’s mobility.
Older people are at most risk of pressure injuries, but they can occur in any patient or in any setting, including:
- acute areas such as operating theatres
- during transportation to a hospital
- intensive care units.
Pressure injuries may impact significantly on a patient’s:
- length of hospital stay
- comfort and quality of life
- cost of care and health outcomes.
Pressure injury-related clinical incidents are those pressure injuries that were not present on the patient’s admission to hospital and are therefore considered hospital-acquired.
How do we measure up
The combined healthcare-acquired pressure injury complications for the NMHS hospitals:
- Sir Charles Gairdner Osborne Park Hospital Care Group
- King Edward Memorial Hospital (Women and Newborn Health Service)
- Graylands Hospital (plus Mental Health and Dental Health)
Chart: Rate of hospital-acquired complications: pressure injury per 1,000 patient days across NMHS, from January to March 2020.
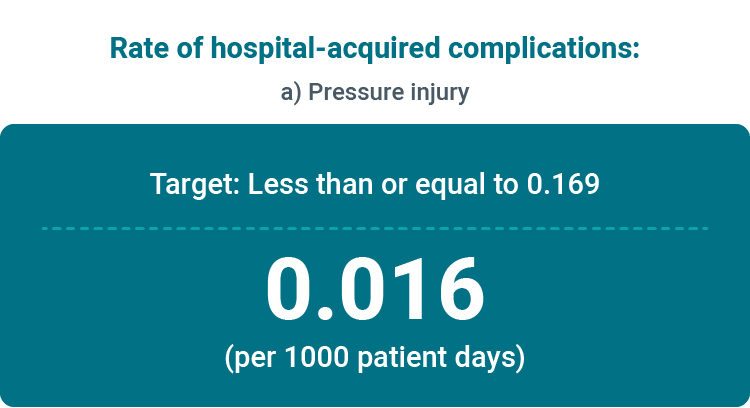
What the figures mean
Pressure injuries are caused by pressure or friction to the skin that causes the skin to tear or breakdown. Incidence of pressure injuries can be reduced by regular repositioning and skin assessments, good nutrition and continence management, and control of comorbidities such as diabetes.
The benchmark for incidence of pressure injuries is less than 0.169 pressure injuries per 1000 patient days. NMHS are consistently performing better than the target.
Hospital-acquired complications – Falls
Each year nearly one quarter of people over 60 years of age will experience a fall. For some people, the injuries caused by their fall may be so serious that they can no longer live independently.
Falls account for over 80 per cent of all injury-related hospital admissions for people aged 65 years and older. They can occur at any age, but the frequency and severity of falls-related injuries increases significantly with age and frailty.
Falls are one of the most frequently reported clinical incidents in hospitals worldwide and are associated with increased:
- length of hospital stay
- care and use of health resources
- discharge rates to a nursing home or residential care facility.
In certain hospital settings, such as rehabilitation, more than 40 per cent of patients with specific clinical problems experience one or more falls during their admission. Of these falls, 30 per cent result in injuries.
How do we measure up
The combined healthcare-acquired falls complications resulting in fracture or intracranial injury for the NMHS hospitals:
- Sir Charles Gairdner Osborne Park Hospital Care Group
- King Edward Memorial Hospital (Women and Newborn Health Service)
- Graylands Hospital (plus Mental Health and Dental Health)
Chart: Rate of hospital-acquired complications: Falls resulting in fracture or intracranial injury per 1,000 patient days, from January to March 2020.
.jpg)
What the figures mean
The benchmark for performance in this area is less than 0.087 per 1000 patient days and we are currently performing better than this target.
What are we doing to improve
Patient falls are one of the most frequently reported incidents throughout hospitals worldwide and can have a significant impact on a patient’s quality of life. Illness and some medications can increase a patient’s risk of falls and so, at NMHS, patients are assessed regularly for their falls risk factors.
To prevent falls and to work towards zero harm from falls, NMHS patients are assessed for the risk of a fall and the potential to be harmed from falls:
- on presentation to hospital
- during their admission
- when clinically indicated.
A combination of falls prevention and harm minimisation strategies are then used for those patients assessed as at risk of falling. These strategies form a falls prevention plan for the patient, and this is monitored regularly to ensure its effectiveness and appropriateness. Patients and carers are also informed of the identified risks from falls and are encouraged to participate in the development of their falls prevention plan.
All patient falls are clinical incidents and require an investigation of causes and contributing factors. Our staff are continuously reviewing and improving strategies to minimise the incidence of falls for our patients.
Hospital-acquired complications – Healthcare-associated infections
Infections people get while being cared for in a healthcare facility are known as healthcare associated infections (HAI).
The most common types of infection acquired in hospitals are:
- urinary tract infection (UTI)
- pneumonia (lung infection)
- wound infection
- bloodstream infection.
For a patient, a HAI can result in:
- illness
- an extended stay in hospital
- a slower recovery
- increased stress
- lower morale.
HAIs are costly to patients, hospitals and the community. While they can occur in any healthcare setting, effective infection prevention and control can significantly reduce the infection rate. Patients, visitors and staff all play a role in reducing HAIs.
How do we measure up
The combined healthcare-associated infections for the NMHS hospitals:
- Sir Charles Gairdner Osborne Park Hospital Care Group
- King Edward Memorial Hospital (Women and Newborn Health Service)
- Graylands Hospital (plus Mental Health and Dental Health)
Chart: Rate of hospital-acquired complications: Healthcare-associated infections per 1,000 patient days, from January to March 2020.
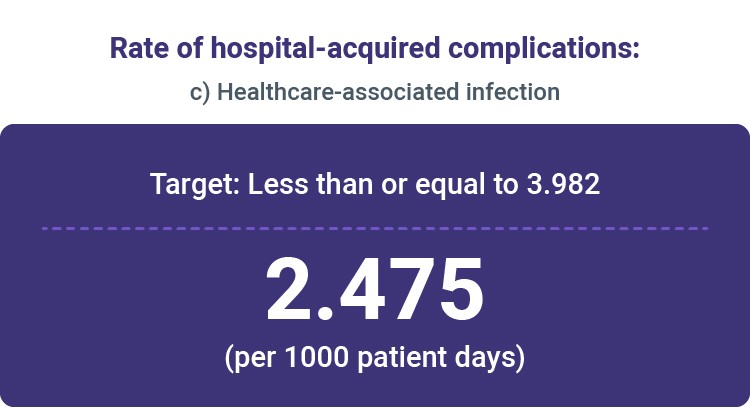
What the figures mean
Infections that are acquired while receiving healthcare can result in a slower recovery. One strategy for preventing infection is for all staff to perform good standards of hand hygiene. At NMHS we regularly audit hand hygiene standards and you can see how we measure up for hand hygiene.
The benchmark for HAIs at NMHS is less than 3.982 per 1000 patient days. Our sites are consistently performing better than the target.
Severity Assessment Code (SAC) 1 clinical incident investigation reporting
When a clinical incident is reported, it is assigned a Severity Assessment Code (SAC) that relates to the level of harm caused to the patient. An incident that results in serious harm or death is allocated a SAC 1 rating and requires a robust investigation by a panel of experts. The report that results from the investigation must be submitted to the Patient Safety Surveillance Unit (PSSU) within 28 days from when the incident was notified.
How do we measure up
The percentage of SAC 1 clinical incidents reported to the PSSU within 28 working days of the event notification date for the NMHS hospitals:
- Sir Charles Gairdner Osborne Park Hospital Care Group
- King Edward Memorial Hospital (Women and Newborn Health Service)
- Graylands Hospital (plus Mental Health and Dental Health)
Chart: Percentage of Severity Assessment Code (SAC) 1 clinical incident investigation reports received by Patient Safety Surveillance Unit within 28 working days of the event notification date, for August 2020.
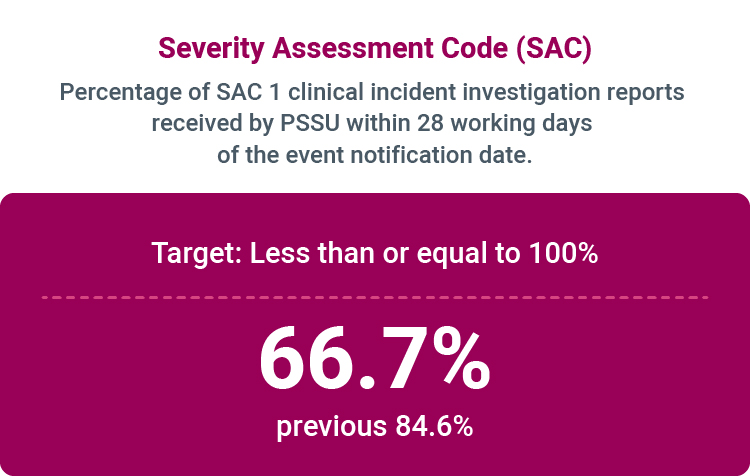
What the figures mean
The target for submission of the report within 28 days is 100% and this graph demonstrates that we are not managing to achieve this target.
What are we doing to improve
NMHS is currently providing training to assist the sites with the Clinical Incident Management process and exploring strategies to improve performance in this area.

