Syphilis outbreak
Syphilis is a bacterial sexually transmitted infection (STI) that can cause a wide range of clinical syndromes, some of which can be severe and long-lasting.
Rates of syphilis infections have been increasing rapidly in WA since 2015, with a syphilis outbreak declared in Perth in July 2020 (Figure 1). Rates are also increasing in regional areas of WA. There were 430 cases of infectious syphilis in Perth in 2023, a four-fold increase since 2015.
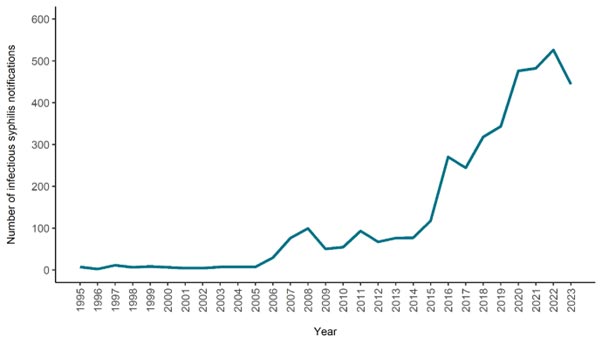
Figure 1: Number of infectious syphilis notifications in metropolitan Perth per year.
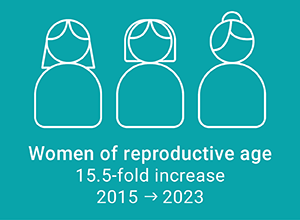
Before the current outbreak, almost all syphilis cases in Perth were reported in gay, bisexual and other men who have sex with men. More recently, there is increasing diversity among cases and priority populations are being impacted.
Priority populations in Perth include women of childbearing age (mostly notably pregnant women), Aboriginal peoples and people experiencing homelessness or unstable accommodation.
A key concern is the potential for congenital syphilis, which is transmitted from mother to fetus in utero. Congenital syphilis is associated with high mortality and morbidity, including miscarriage and stillbirth, skeletal changes and other organ effects.
Congenital syphilis is preventable. If the mother is treated 30 days or more before giving birth, it can significantly reduce the risk.


General information on syphilis can be found at HealthyWA website (external site), or information about the state-wide response is available via WA syphilis outbreak response (external site).
Current state-wide notification data is available on the national infectious disease dashboard (external site). Information in relation to the national response is available on the national response to syphilis website (external site).
The clinical presentation of syphilis is described on the WA Department of Health Silver Book (external site).
Key recommendations for clinicians
Testing
Populations recommended to receive regular screening for syphilis include:
- any person with a new sexual partner
- gay, bisexual and other men who have sex with men
- Aboriginal and Torres Strait Islander peoples
- people who use methamphetamine and IV drugs
- people experiencing homelessness or unstable accommodation
- sex workers.
Helpful guides on interpretation of syphilis test results have been developed by ASHM, as part of the decision making in syphilis tool (PDF) and the syphilis outbreak training website (external site).
Treatment
The main treatment for syphilis is long-acting benzathine benzylpenicillin, given intramuscularly. The treatment depends on clinical staging.
|
Stage |
Recommended dose of benzathine benzylpenicillin |
|
Infectious syphilis (primary, secondary, early latent) |
2.4 million units (two syringes/vials), stat |
|
Non-infectious syphilis (late latent) or syphilis of unknown duration |
2.4 million units (two syringes/vials), given one week apart over two weeks i.e., Day 0, 7 and 14 (total three doses) |
Benzathine benzylpenicillin is not readily available from community pharmacies but can be ordered through the prescriber bag website (external site). Practices are recommended to keep this in stock to facilitate prompt management.
There have been interruptions to supply of the preferred brand of benzathine benzylpenicillin, Bicillin L-A. Current information is available from the TGA (external site). Practices in the Perth metropolitan area who require an urgent supply of benzathine benzylpenicillin should contact Boorloo PHU.
People with penicillin hypersensitivity should speak with a sexual health physician in relation to desensitisation options, or alternatives to penicillin.
Syphilis in pregnancy
A diagnosis of syphilis in pregnancy requires accurate management and close follow-up, to prevent congenital syphilis. It is recommended that initial management is discussed with a sexual health physician, clinical microbiologist, or an infectious diseases specialist. Women with infectious syphilis who are more than 23 weeks' gestation should receive treatment under inpatient monitoring (PDF) because of the risk of pre-term contractions due to Jarisch-Herxheimer reactions.
The Syphilis Response Team (SRT) located at Boorloo PHU specialises in coordinating the follow-up of women who have received treatment for syphilis during pregnancy. The SRT conducts monthly case review meetings where management plans are discussed with a multi-disciplinary team, including antenatal care providers, sexual health physicians, clinical microbiologists and infectious diseases specialists.
The Syphilis Response Team (SRT) can be contacted during office hours.
Syphilis resources
Syphilis testing in pregnancy poster (PDF)
Syphilis testing in pregnancy - Patient information (PDF)
Congenital syphilis flyer (PDF)
ASHM - Decision Making in Syphilis (PDF)
NMHS Women and Newborn Health Service - Statewide Maternity Shared Care Guidelines (PDF)
NMHS Women and Newborn Health Service - Syphilis in Pregnancy (clinical practice guideline) (PDF)
WA Health - Silverbook, Syphilis (external site)
ASHM - Interactive Syphilis Tool (external site)
RACGP – Video guide on injecting Bicillin-LA in the ventrogluteal space (external site)
Clinicians can request a free education session for their unit or practice from a member of the specialist Syphilis Response Team (SRT) in relation to testing, treatment, syphilis in pregnancy or other syphilis-related queries.
Please contact srt.bphu@health.wa.gov.au for more information.
Syphilis education and training
RACGP - Syphilis outbreaks in WA (external site)
ASHM - Syphilis Outbreak Training (external site)
WAPHA seminars for STI testing and management (external site)