Return to activity considerations
 Driving
Driving
There are no legal requirements regarding returning to driving following a concussion or mild head injury, as the expectation is that the majority of people will return to all previous activities with little to no changes in performance within a week or a few weeks. If you have presented to ED or your GP, they may recommend a limited time of not driving based on the symptoms you present with.
These symptoms may include:
- Reduced concentration
- Reduced rate of thinking and responding
- Headaches and fatigue
- Dizziness
- Overstimulation from fast moving environment
- Poor visual tracking
- Intolerance to noise and light.
Some people post-concussion report a loss of confidence and capacity to manage driving safely at night, in busy / fast environments, when under time pressures, when reversing and when fatigued.
It is important to maintain safe driving practices such as:
- Choosing not to drive at night
- Practice skills in quieter environments initially
- Starting with short / local trips
- Initially returning to driving with someone else in the car
- Reduce any additional demands or distractions when driving (eg passengers don’t talk, music is off)
- No time pressures
- Plan ahead (ie Time it will take you at the time of day to get to your appointment and add on more time than necessary, visualize the route in your head or on your phone prior to the trip).
If you do present with persisting symptoms your doctor may recommend for you to have an on-road occupational therapy driving assessment prior to commencing driving.
 Return to study protocol
Return to study protocol
Allow 24 hours as a minimum between stages 1 to 3 and 1 to 2 weeks as a minimum between stages 4 to 6, if symptom free. Go back one step if symptoms resume.
| Stage | Functional exercise | Objective |
| 1. No activity | Complete cognitive rest | Recovery |
| 2. Minor cognitive activity at home | Short periods (5 to 15min) of cognitive activity (homework) | Gradual, closely monitored increase in sub symptom threshold activities |
| 3. Moderate cognitive activity at home | Longer periods (20 to 30mins) of cognitive activity (homework) | Increase cognitive stamina, self paced activity |
| 4. Partial school entry | Part day of school attendance, plus 1 to 2 cumulative hours of homework | Re-entry into school with accommodation to maintain cognitive load below symptom threshold |
| 5. Gradual reintegration to school | Gradual increase to full day of school attendance | Increase cognitive stamina, gradual decrease of accommodations |
| 6. Full cognitive workload resumed | Catch up on essential missed work, re-introduce testing and assessments | Full return to school, recommended to commence RTP protocol |
 Return to work protocol
Return to work protocol
Allow 24 hours as a minimum between stages 1 to 3 and 1 to 2 weeks as a minimum between stages 4 to 6, if symptom free.
| Stage | Functional exercise | Objective |
| 1. No activity | Complete cognitive rest (Maximum of 1 to 2 days). | Recovery |
| 2. Minor cognitive activity and light aerobic exercise in/around home | Short periods (5 to 15min) of cognitive activity (texting / computer) and going for walks up to 10 to 15 minutes, simple chores. | Gradual, closely monitored increase in sub symptom threshold activities |
| 3. Moderate cognitive / physical activity in / around home | Longer periods (20 to 30mins) of cognitive activity (social media / TV) or housekeeping tasks. | Increase cognitive / physical stamina, self paced activity |
| 4. Part time work | Part day in work environment, consider 3 mornings a week (ie Monday, Wednesday, Friday) for 3 to 4 hours. Ensure one task at a time. | Re-entry into work environment with accommodation to maintain cognitive load below symptom threshold, commence GRTWP |
| 5. Gradual reintegration to work | Gradual increase to full work days (ie Monday, Wednesday, Friday), then onto a full working week with reduced responsibilities, time pressures and restricted duties. | Increase cognitive stamina, gradual decrease of accommodations, progress GRTWP |
| 6. Full time work and duties | Catch up on essential missed work, and plan out priorities. | Full return to work |
 Return to sport protocol
Return to sport protocol
Allow 24 hours as a minimum between each stage, if symptom free. Go back one step if symptoms resume.
| Stage | Functional exercise | Objective |
| 1. No activity | Complete physical and cognitive rest. | Recovery |
| 2. Light aerobic exercise | Walking, swimming or stationary cycling for 10 to 15 minutes, keeping intensity <70% maximum permitted heart rate. Avoid resistance training and other heavy lifting. | Increase heart rate |
| 3. Sport specific exercise | Running and throwing drills. Avoid body contact, resistance training, heavy lifting and other jarring motions. | Add movement |
| 4. Non contact training drills | Progression to more complex training, eg passing / press drills. Start progressive resistance exercises but avoid impact activities. | Exercise, coordination and cognitive load |
| 5. Full contact practice | Following medical clearance, return to normal training activities. | Restore confidence and assess functional skills |
| 6. Return to play | Normal game play. | Full return to pre-concussion activities |
Return to work considerations
Open return to work considerations page.
Community education and support
In between the ears is a WA support link that provides quality education and support regarding the effect’s concussion can have. They can provide an educational presentation to sporting clubs, schools and organisations where they speak about their personal experiences and struggles with concussion. They have linked with the leading concussion specialists, here in WA, to help provide the latest research and science. See In between the ears (external site) for more information.
 Exercise and activity post-concussion
Exercise and activity post-concussion
The best way to assist the body to regulate itself again post-concussion is through a graded return to activity.
- After the initial 24 to 48 hours relative rest period, it is important to resume gentle activity and movement. This helps give gentle exposure to external environments (eg lights, noise, movement) and can help with mood and mental health.
Doing too little initially, or pushing too much too soon can delay recovery.
- Post-concussion the body’s autonomic nervous system regulation can be impacted. The autonomic nervous system is responsible for regulating key involuntary functions including heart rate, blood pressure, breathing, digestion and gland secretion.
- Too little: The body needs some regular activity to gently challenge these systems and promote normal regulation. Extended rest leads to deconditioning (losing fitness) which can mean easier irritation of symptoms and can prolong symptoms such as fatigue, sleep disturbance and irritability.
- Too much: If pushed too hard too early you may get irritation of your symptoms (eg headache, dizziness or fogginess) as the systems get over loaded and struggle to regulate themselves.
The aim is to find the sweet spot doing as much as you can with minimal symptoms.
- As a general activity guide, initially aim for 15 to 20 minutes of gentle walking or low-grade cardio daily and gradually build from there. If this is too much at once, break into smaller timeframes throughout the day and gradually work up.
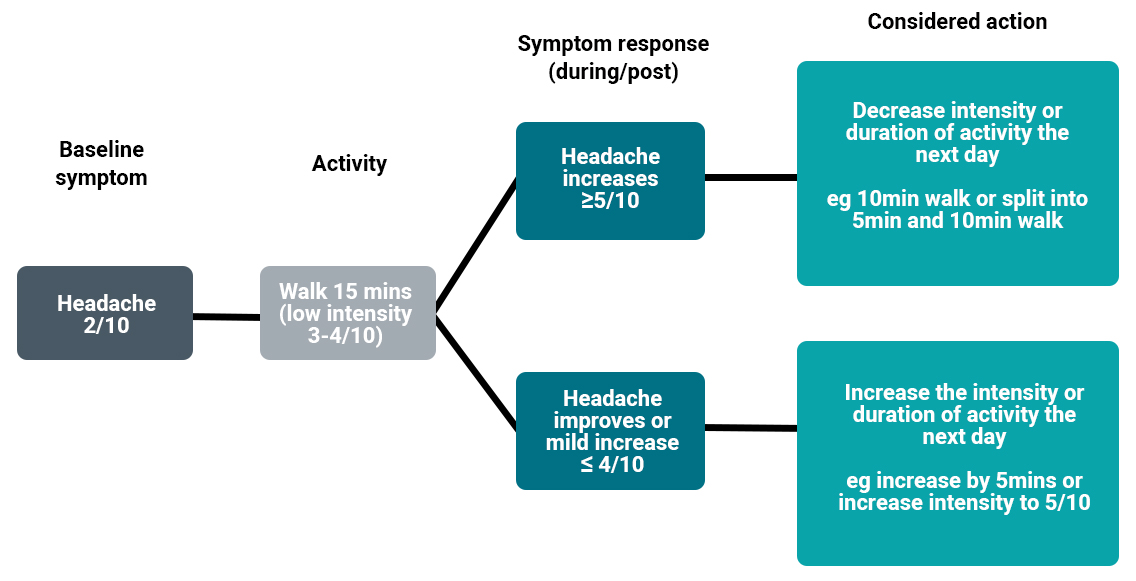
- It can be useful to score your symptoms on a 0 to10 scale prior to activity and consider the +3 rule.
- If your score increases by 3 or more during the activity, the intensity or duration should be temporarily lowered to a manageable level.
- If your score increases by less than 3 or improves during activity, you can step up the intensity or duration the following day.
- If your symptoms at base line are limiting you from participating in regular activity review by your GP / health care provider is recommended to provide further guidance and enable you to return to activity
If you continue to have ongoing symptoms and / or you are returning to sport or other high-level activities (eg sports, military duty, manual labour) it is recommended you see a physiotherapist experienced with concussion to assess your readiness to return to your chosen activity. Trained therapists can assess your response to exertion using tests such as the Buffalo Concussion Treadmill Test (BCTT) and, based on these results, prescribe a tailored exercise program for you.
- For a general guide to return to sports and higher-level activity see return to sports protocol.

